Submitted on Monday 1st October 2018
Published on Tuesday 23rd October 2018
Current status: Closed
Closed: Tuesday 23rd April 2019
Signatures: 10,876
Tagged with
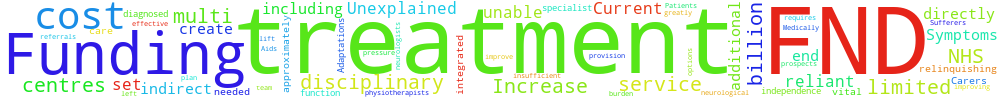
Increase funding for multi-disciplinary treatment centres for FND Patients.
Funding is needed to set up and increase service provision for multi-disciplinary treatment centres. Treatment requires specialist care with a team of neurologists, physiotherapists etc. which must be integrated to create an effective plan. Current options are limited & insufficient.
Up to 1/3 of all neurological referrals are diagnosed with FND. Sufferers end up relinquishing their independence & become reliant on Carers, Aids and Adaptations. They are left unable to function & it’s vital we improve prospects. Medically Unexplained Symptoms (including FND) directly cost the NHS approximately £3.1 billion, with an additional £18 billion in indirect costs. With an NHS already under pressure, improving services and treatment for those with FND would greatly lift this burden.
You can't sign this petition because it is now closed. But you can still comment on it here at Repetition.me!
The Government responded to this petition on Monday 29th April 2019
The funding and planning of services for patients with FNDs is a local matter. Patients with FND should receive appropriate assessment and support with access to specialists as appropriate.
The Government recognises functional neurological disorders (FNDs) can be a great source of distress for patients and can have a significant impact on their quality of life. Population prevalence estimates for FND vary, suggesting incidence could be between 4 and 12 per 100,000. Patients with FND can present with a wide range of symptoms, including; limb weakness and paralysis, chronic pain, numbness, loss of consciousness and cognitive and visual disturbances. These could suggest an underlying neurological condition, but in patients with FND these symptoms are not explained by any neurological disease, and the exact cause of FND is not known. Because of this, FND is identified by the exclusion of such underlying neurological disorders, and it can sometimes take some time for these other serious neurological diseases to be ruled out. Sometimes the symptoms resolve, but for others the condition is long lasting.
As with the majority of NHS services, the funding and planning of services for patients with functional neurological disorders (FNDs) is a local matter. Local NHS Commissioners are best placed to design services for their resident populations, supported by relevant clinical guidance where available. Patients presenting with neurological symptoms should receive appropriate management and referral to a neurologist for assessment and investigation, if appropriate. Whether a patient is under the care of a secondary care neurology service or under the care of a GP, management of FND may require input from a range of professionals, either via direct referral or as part of multidisciplinary team care.
There no one single approach to managing patients with FND. Treatment may involve drugs to manage specific symptoms, physiotherapy, occupational therapy, rehabilitation care and psychological support. All people with long term health problems, including those identified as having FND, should receive a care plan to support their care, treatment and support. This process recognises the person’s skills and strengths, as well as their experiences and the things that matter the most to them. It addresses the things that aren’t working in the person’s life and identifies outcomes and actions to resolve these though an individualised approach. Care plans have long been the basis of the approach to long-term condition (LTC) management and NHS England has recently announced plans to step up its approach. On 31 January 2019 NHS England launched the Comprehensive Personalised Care model, and it has committed to roll out the model across the country, reaching 2.5 million people by 2023/24. The model, which includes self-care, personalised care planning, personal health budgets and social prescribing, is particularly relevant to people with long term conditions. Self-management approaches, in particular, can be useful in helping patients manage day to day symptoms and improve quality of life. The model is now being implemented across a third of England. By September 2018, over 200,000 people had already joined the personalised care programme.
The use of cognitive behavioural therapy (CBT) has shown to be beneficial in managing FND. On the 21 March 2018 NHS England and NHS Improvement along with the National Collaboration Institute for Mental Health published ‘The IAPT Pathway for People with Long-term Physical Health Conditions and Medically Unexplained Symptoms’ (MUS). IAPT services provide evidence based treatments for people with anxiety and depression. The guidance outlines the IAPT pathway, and accompanying benchmarks, to support the national expansion of IAPT services such CBT, for adults with LTCs and MUS.
This expansion will see IAPT services co-located in existing primary and secondary care physical health pathways. NHS England is committed to continue improving access to IAPT services for adults with common mental health problems, with a focus on those with LTCs. The NHS Long Term Plan set out that by 2023/24, an additional 380,000 adults will be able to access IAPT services.
Finally, you may be interested to know that the National institute for Health and Care Excellence, which provides evidence based guidance to the NHS, is in the process of developing the clinical guideline Suspected neurological conditions: recognition and referral. The scope of the guideline includes looking at aspects of functional symptoms.
Department of Health and Social Care.
18.227.105.41 Sun, 23 Feb 2025 19:39:31 +0000