Submitted on Thursday 25th April 2019
Published on Thursday 30th May 2019
Current status: Closed
Closed: Wednesday 6th November 2019
Signatures: 29,336
Tagged with
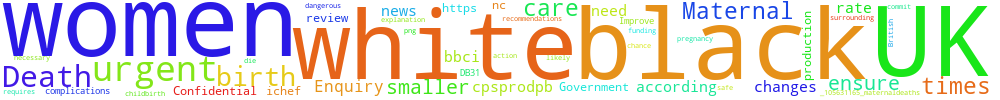
Improve maternal care for black British women
Black women in the UK are five times more likely to die from complications surrounding pregnancy and childbirth than white women. We need an urgent review of care with recommendations on how to ensure it is no more dangerous for black women to give birth in the UK than white women.
The Government must commit to funding the changes necessary to ensure it is safe to give birth while black in the UK. The chance of death is 1 in 2,500 for black women according to the UK Confidential Enquiry into Maternal Deaths . But the rate was five times smaller for white women between 2014 and 2016. This requires urgent explanation and action.
https://ichef.bbci.co.uk/news/695/cpsprodpb/DB31/production/_105631165_maternaldeaths-nc.png
You can't sign this petition because it is now closed. But you can still comment on it here at Repetition.me!
The Government responded to this petition on Tuesday 22nd October 2019
The Government is funding research at the Maternal and Neonatal Health and Care PRU to investigate the factors associated with the excess risk of maternal death for Black and South Asian women.
Analysis of maternal deaths, stillbirths and neonatal deaths, undertaken by MBRRACE-UK (Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries across the UK) at the University of Oxford, shows that poor outcomes are much higher for mothers and babies from Black/Black British and Asian/Asian British ethnic groups and women living in the most deprived areas of the country.
Black women are five times more likely to die from causes related to pregnancy than white women. Black babies have a 121% increased risk for stillbirth and a 50% increased risk for neonatal death (i.e. dying within 28 days after birth) compared to white babies. Asian women are twice as likely to die from causes related to pregnancy than white women. Asian babies have a 55% increased risk for stillbirth and a 66% increased risk for neonatal mortality compared to white babies. Babies born to mothers in the most deprived areas of the country have a 30% increased risk neonatal mortality. For all of these groups the risk of a poor pregnancy outcome compared to white women or women in less deprived areas is increasing.
The NHS Long-Term Plan takes a concerted and systematic approach to reducing health inequalities and addressing unwarranted variation in care. The Chief Midwifery Officer, Professor Jacqueline Dunkley-Bent OBE, is leading work to support maternity services to provide high-quality maternity care for all women with a scale and intensity that is proportionate to the level of disadvantage (known as ‘proportionate universalism’). Initiatives recently introduced to reduce and eliminate health inequalities in maternity include:
• Targeted and enhanced continuity of carer – Evidence suggests that continuity of carer can significantly improve outcomes for women from ethnic minorities and those living in deprived areas. The NHS Long-Term Plan describes how an enhanced and targeted continuity of carer model is being implemented to help improve outcomes for the most vulnerable mothers and babies. Continuity of carer teams are being developed and launched across the country with the aim that in 2019, 20% of pregnant women will be offered the opportunity to have the same midwife caring for them throughout their pregnancy, during birth and postnatally. We will continue to work with midwives, mothers and their families to implement continuity of carer so that, by March 2021, most women receive continuity of the person caring for them during pregnancy, during birth and postnatally. This will be targeted towards women from Black and Minority Ethnic (BAME) groups and those living in deprived areas, so that by 2024, 75% of women from BAME groups and a similar percentage of women from the most deprived communities will receive continuity of carer from their midwife throughout pregnancy, labour and the postnatal period. This will help reduce pre-term births, hospital admissions, the need for intervention during labour, and women’s experience of care.
• The NHS Planning Guidance 2019/20 sets an expectation that local systems will to start to implement continuity of carer models for Black and Asian women and those in the most deprived areas.
• The Department of Health and Social Care is funding research through the National Institute of Health Research’s Policy Research Unit (PRU) in Maternal and Neonatal Health and Care at the University of Oxford to investigate the factors associated with the excess perinatal mortality experienced by BAME babies; and identify the factors associated with the excess risk of maternal death for Black and South Asian women.
• Improving ethnic coding in maternity data systems - Ethnic coding data is not present for 16% of Maternity Services Dataset records. We will work with NHS Resolution to include an effective incentive to improve coding completeness in the Maternity Safety Incentive Scheme in future years.
• Health Safety Investigation Branch (HSIB): learning from parents - Work is underway with HSIB to learn from their interviews with parents, including an analysis by ethnicity and deprivation index.
• Gap analysis for each workstream of the Maternity Transformation Programme - We are working with NHS England / NHS Improvement and other system partners to map current work and additional actions and support that may be needed to reduce and eliminate inequalities.
• Measurement - Health inequality measures covering a range of clinical quality indicators have been developed as part of the NHS Long-Term Plan work.
Department of Health and Social Care.
This is a revised response. The Petitions Committee requested a response which more directly addressed the request of the petition. You can find the original response towards the bottom of the petition page (https://petition.parliament.uk/petitions/259256)
3.143.254.39 Mon, 03 Mar 2025 19:51:55 +0000