Submitted by Atinuke Awe on Monday 9th March 2020
Published on Friday 13th March 2020
Current status: Closed
Closed: Sunday 13th September 2020
Signatures: 187,520
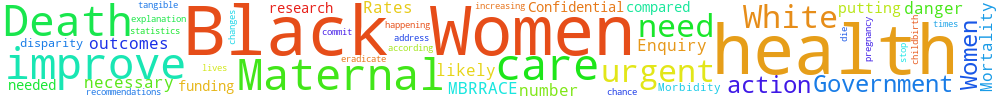
Improve Maternal Mortality Rates and Health Care for Black Women in the U.K.
Black Women in the U.K. are 5 times more likely to die during pregnancy and after childbirth compared to White Women (MBRRACE, 2019). We need more research done into why this is happening and recommendations to improve health care for Black Women as urgent action is needed to address this disparity.
The Government must commit to funding the changes necessary to eradicate these statistics and improve maternal health care outcomes for Black Women.
Between 2015-2017 the chance of death for Black Women was 38 out of 100,000 however it was 7 out of 100,000 for White Women according to the Confidential Enquiry into Maternal Deaths and Morbidity.
An urgent explanation and tangible action needs to be done by the Government to stop this number increasing and putting Black Women’s lives in danger.
You can't sign this petition because it is now closed. But you can still comment on it here at Repetition.me!
The Government responded to this petition on Thursday 25th June 2020
The Government is funding a NIHR Policy Research Unit in Maternal and Neonatal Health and Care study into factors associated with the higher risk of maternal death for Black and South Asian women.
Analysis of maternal deaths, stillbirths and neonatal deaths, undertaken by MBRRACE-UK (Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries across the UK) at the University of Oxford, shows that poor outcomes are much higher for mothers and babies from Black/Black British and Asian/Asian British ethnic groups and women living in the most deprived areas of the country.
The NHS Long-Term Plan
The NHS Long-Term Plan (LTP) takes a concerted and systematic approach to reducing health inequalities and addressing unwarranted variation in care. Work to improve equity in health outcomes for mothers and their babies is led by Professor Jacqueline Dunkley-Bent OBE, Chief Midwifery Officer for England. The work aims to understand why mortality rates are higher, consider evidence about what will reduce mortality rates and take action to improve equity in outcomes for mothers and their babies. This is being carried out as part of the Maternity Transformation Programme (MTP), which is implementing the vision for maternity services set out in ‘Better Births’ and the NHS LTP.
The MTP works through Local Maternity Systems, which bring together service users, commissioners, and provider trusts to design and deliver maternity services. They are well placed to ensure that services meet the needs of diverse local communities. The LTP committed to implementation of an enhanced and targeted continuity of carer model for Black, Asian and minority ethnic (BAME) women, as well as for women from the most deprived areas. By 2024 75% of women from BAME background will receive continuity of care from their midwife throughout pregnancy, labour and the postnatal period, with additional midwifery time where needed. The evidence shows that continuity of carer models helps reduce pre-term births, hospital admissions, the need for intervention during labour, and to improve women’s experience of care. Continuity of carer can significantly improve outcomes for women and their babies from ethnic minorities and those living in deprived areas
Local Maternity Systems will receive funding and support to implement targeted and enhanced continuity of carer from 2021. In the meantime, Local Maternity Systems are rolling out a standard continuity of carer model and the NHS Planning Guidance 2019/20 stated that that they should use all reasonable endeavours to prioritise women who face the poorest outcomes, which includes BAME women.
The MTP is promoting greater service user participation in the design and delivery of maternity services through Maternity Voices Partnerships (MVPs), and is making particular efforts to ensure diverse voices are heard. National Maternity Voices, funded by NHS England and NHS Improvement, are providing additional support for BAME parent representatives.
Responding to the Coronavirus pandemic
DHSC is funding studies through the National Institute for Health Research (NIHR) – funded Policy Research Unit in Maternal and Neonatal Health and Care, at the University of Oxford, to identify the factors associated with the higher risk of maternal death, and more recently to provide data on the impact of the SARS-CoV-2 pandemic on BAME pregnant women.
The UK Obstetric Surveillance System collects information about all pregnant women admitted to hospital who are confirmed to have the virus infection including the influence of demographic characteristics on outcomes for mother and infant. This research group published a paper in the British Medical Journal (BMJ) on 8 June 2020, Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population-based cohort study, which states that 56% pregnant women admitted to hospital with SARS-CoV-2 infection in pregnancy were from black or other ethnic minority groups.
The Chief Midwifery Officer has written to Local Maternity Systems, asking them to take specific actions which will minimise the additional risk of COVID-19 for BAME women and their babies. These include local systems increasing support for BAME pregnant women through co-production and implementation of an operational policy for how they will manage the risks of COVID-19 for pregnant women from a BAME background and tailored communications for pregnant BAME women with information about local services and to reassure them that maternity services are available during the pandemic, and encourage them to seek help if they have any concerns.
Department of Health and Social Care
This petition has reached the threshold for a Parliamentary debate, but the debate has not yet been scheduled.
52.15.73.53 Sat, 22 Feb 2025 16:43:09 +0000