Submitted by Rebecca Thomas on Wednesday 24th August 2022
Published on Wednesday 31st August 2022
Current status: Closed
Closed: Tuesday 14th March 2023
Signatures: 13,208
Relevant Departments
Tagged with
Breathe ~ Covid ~ Covid-19 ~ disease ~ Equal ~ Europe ~ Improved ~ investment ~ KILLS ~ People in the UK ~ Permanently ~ Post Covid ~ Ratings ~ risk
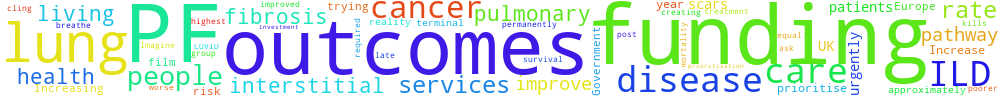
Increase funding for treatment of pulmonary fibrosis & interstitial lung disease
We ask the Government to prioritise funding for PF and interstitial lung disease services. PF is terminal and kills approximately 8,000 people a year. It has a survival rate worse than many cancers. Increasing funding and creating a care pathway equal to cancer care could improve health outcomes.
Imagine trying to breathe through cling film. This is the reality for many of the 70,000 people in the UK living with PF - a group of 200+ diseases that permanently scars lungs.
The UK has one of the highest mortality rates in Europe for ILD and pulmonary fibrosis patients are at risk of poorer health outcomes post COVID-19.
Investment and prioritisation of funding for ILD services is required urgently. An improved PF care pathway could improve outcomes for patients living now, before it’s too late.
You can't sign this petition because it is now closed. But you can still comment on it here at Repetition.me!
The Government responded to this petition on Wednesday 1st February 2023
NHS England commissions services for interstitial lung disease (ILD) and funds the cost of treatments. Access to treatments has been expanded to patients with non-idiopathic pulmonary fibrosis.
NHS England is responsible for the commissioning of services for interstitial lung disease (ILD) and funds the cost of anti-fibrotic treatments to treat this disease. Access to these treatments has recently been expanded to patients with non-idiopathic pulmonary fibrosis following the publication of the National Institute for Health and Care Excellence’s technology appraisal ‘Nintedanib for treating progressive fibrosing interstitial lung diseases’ in November 2021.
NHS England’s service specification outlines the requirements of a quality service and requires the completion of metrics through the ILD Specialised Services Quality Dashboard. The Specialised Respiratory Clinical Reference Group contains clinical members who advise NHS England on ILD services and includes a member of a pulmonary fibrosis charity as a patient and public voice member. It is expected that commissioning responsibility for these services will be delegated by to integrated commissioning boards with effect from April 2023, while NHS England will retain responsibility for setting national standards.
Patients with pulmonary fibrosis are cared for by regional specialist Interstitial Lung Disease services. These are commissioned by NHS England. In order to be referred to a specialist service patients need to be identified in primary and secondary care. Early and accurate diagnosis is a priority for NHS England, and the work to improve this area of clinical care is underway, which should have an impact on reducing delayed diagnosis of pulmonary fibrosis.
This work is as follows:
• The respiratory interventions proposed in the NHS Long Term Plan (LTP) include early and accurate diagnosis of respiratory conditions. To deliver this LTP commitment NHS England has established 13 Respiratory Clinical Networks across the country.
• Spirometry is one of the tests used to diagnose pulmonary fibrosis.
• Through the NHS’s annual priorities and planning guidance, systems have been asked to work towards restoring spirometry checks for adults and children to pre-pandemic levels in 2022/23. The importance of restoring spirometry has also been reaffirmed in the delivery plan for tackling the Covid-19 backlog of elective care. The Respiratory Clinical Networks have been vital in providing clinical leadership for respiratory services and supporting services in the restoration of spirometry in primary care.
• Diagnosis is also being incentivised within the Quality Outcomes Framework for 2022/23 which includes respiratory indicators in relation to the diagnosis of asthma and COPD which was fully re-instated in April 2022.
• Community Diagnostic Centres (CDCs) are being established to deliver additional, digitally connected, diagnostic capacity in England, providing patients with a coordinated set of diagnostic tests in the community, in as few visits as possible, enabling an accurate and fast diagnosis on a range of clinical pathways including pulmonary fibrosis.
• As part of this, a pathway for the diagnosis of undifferentiated breathlessness is being piloted in a small number of CDCs with a view to wider rollout.
• Breathlessness is a common presenting symptom in primary care with numerous causes. A delayed or inaccurate diagnosis means people don’t get the treatment they need and can end up in hospital unnecessarily. There is rarely a single cause of breathlessness, therefore, multiple investigations are likely to be required and a holistic approach needed.
Department for Health and Social Care
18.119.133.172 Sat, 18 Jan 2025 00:42:20 +0000